Men remain as vulnerable as women, if not more, with regards to health problems involving their genital and urinary system. One saving grace for men is that almost all parts of their genital system with the exception of prostate gland are accessible to self-assessment by the man; unlike women with hidden genitals making their self- assessment and clinical examination rather difficult.
So what do men need to do to ensure they remain healthy or trouble free: get themselves an MOT, which would involve self-assessment and check ups with GPs / specialists at regular intervals depending upon their respective ages; irrespective of any leading symptoms.
What are the common urinary symptoms men present to their GPs / Specialists with?
- Difficulties with urination namely:
- Night time frequency and slow urine flow
- Urinary incontinence particularly bed wetting at night Blood in the urine
- Painful urination
- Fever (>38 degree C) with chills with / without flank pain
What are these symptoms commonly related to?
These symptoms are related to benign enlargement of prostate (BEP) gland. Prostate is a part of male reproductive system, contributing to semen and that all men have at the base of their bladder. It is an age related common occurrence, with over 50 % of men above the age of 40 yrs requiring some form of intervention for it.
Of note, is the seriuous element attached to the presence of visible blood in the urine (Haematuria) with or without the prostate symptoms, which warrants thorough investigations including a kidney scan (Ultrasound or CT) and a camera examination of the bladder (cystoscopy) to rule out the Big C in the urinary tract (Kidney / bladder)
How do you assess your prostate gland?
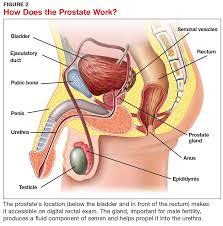
The simple answer is that you your self cannot; as it remains inaccessible to self-assessment, situated deep down in the pelvis, but just beneath the bottom/buttock that you sit on and hence the importance of having it checked out by your GP / Specialist when urination becomes an issue.
Digital rectal examination (DRE) of the prostate, preformed by putting a finger up the anus / back passage, has an accuracy of only 40 % in making a diagnosis of prostate cancer but is also extremely helpful in making a clinical diagnosis of prostatitis, an inflammatory condition of the prostate, with or without associated bacterial infection and in clinical practice more commonly seen than prostate cancer, especially in the age group of 18 – 40 yrs.
How about getting a routine blood test for checking on one’s prostate?
Prostate specific antigen (PSA) is a commonly performed blood test for assessment of prostate both by GPs and Specialists, but is not an ideal screener for prostate cancer, with an accuracy reaching only 30% since many other prostatic diseases apart from prostate cancer can influence its levels. It should only be done when deemed appropriate by your GP / Specialist.
It is certainly has value as a screening test in making an early diagnosis of prostate cancer particularly in those men with strong family history of prostate cancer in one or more first-degree relatives and that too especially in those whose relatives have had their prostate cancer diagnosed at a younger age of < 55 yrs, with a possible genetic link.
Multi-Parametric Magnetic Resonance Imaging (MP-MRI) scan with technological advances has been more accurate (85%) in diagnosing prostate cancer but again is to be considered following an initial clinical assessment and an abnormal / elevated PSA (> 3 mcg/l as per new guidelines). However, a final diagnosis of prostate cancer can only be reached after subjecting an individual with abnormal DRE, abnormal PSA and an abnormal MP-MRI score, to systematic biopsies of the prostate and the biopsies returning positive for prostate cancer. If the biopsies return negative, cancer cannot be confidently ruled out in such cases.
Can prostate biopsies be avoided?
In recent years, with increasing accuracy of MP-MRI scan in ruling out clinically significant prostate cancer, biopsies can be avoided in select cases when the Likert score on the MP-MRI is 3 or below but with scores of over 3, a biopsy of the prostate is warranted to confirm cancer.
What other symptoms are relevant to male genito – urinary system that men should be alert about apart from the prostate related symptoms?
A palpable lump involving a testicle, particularly if it is painless, needs an urgent clinical assessment to rule out testicular cancer. The incidence of testis cancer is at its peak between the ages of 15 – 35 yrs but of course, is also seen in men above 35 yrs, albeit less frequently.
Rarely, painful testicular lumps can also turn out to be sinister and warrant an urgent ultrasound scanning after an initial clinical assessment by a GP / Specialist.
What does acute onset testicular pain mean?
Of note is the importance of severe, acute onset, one- sided testicular pain particularly with adolescents, indicates testicular torsion unless proved otherwise. It requires an urgent clinical assessment in a nearby A/E or by a GP / Specialist to rule out a twisted testicle; as it needs to be surgically untwisted within 6 – 8 hrs or else it could suffer irreversible damage and one may lose it both physically and / or functionally for good with long term implications on fertility.
Is there anything to look out on the penis that warrants urgent attention?
Red patches on the head of the penis (glans penis), which fail to clear with local application of various creams that your GP may prescribe, warrants a specialist’s attention as it may require a biopsy to rule out a sinister problem.
A palpable lump on the penile shaft, particularly associated with awkward, painful bending of the penis on erection, indicates a relatively uncommon condition called Peyronie’s deformity (seen in 3-10% men) and needs a Specialist’s review to assess its severity and for the individual to understand its natural history and various options available for treating it. Men need not suffer in silence from this worrisome condition, which can destroy one’s body image and sexual confidence, but explore ways of addressing it actively.
However, a painless lump on the head or shaft of the penis not associated with bending on erection is more likely to be sinister than the painful one and needs urgent attention to rule out the Big C.
Has a man’s failing sex life anything to do with his heart?
An important message for future is that there is a well-established link between male genital disorders such as erectile dysfunction (ED), testosterone deficiency syndrome (TDS) and a man’s heart or cardiovascular system, meaning coronary artery / heart disease.
More on that in my next blog……

Mr. Sudhanshu Chitale
Consultant Urological Surgeon, Whittington Hospital
Honorary Clinical Associate Professor
UCL Medical School, London
For appointment:
Urologysecretary.sc@gmail.com
Tel: 07979 143368
Private Practices:
The London Clinic,
116, Harley Street,
London
W1G 7JL
47, Nottingham Place,
London
W1U 5NY
Wellington Diagnostic Centre, 296, Roman House, Golders Green Rd,
London
NW11 9PY
Highgate Hospital, 17-19, View Rd, Highgate, London
N6 4DJ
BMI – Kings Oak Hospital, Chase Farm North Side, The Ridgeway, Enfield,
London
EN2 8SD