A middle-aged patient in my clinic might have slipped and fallen on their outstretched hand. After six weeks in plaster for a broken wrist a good friend suggested they may have osteoporosis, needed to have a bone density scan and to see a rheumatologist.
Rheumatologists are a mysterious crowd. Our responsibility includes illness relating to joints such as rheumatoid arthritis, osteoarthritis and gout but we also look after conditions which do not fit elsewhere. One grey area is bone health and osteoporosis in particular.
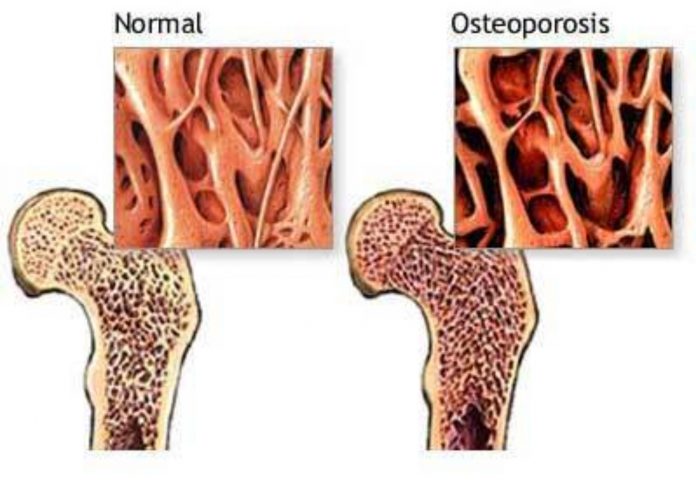
Bone is complex, structured like a firm sponge. As we mature our bones strengthen, achieving as young adults what is called peak bone mass. Bone then remains strong because we produce and absorb it in balance. In later life, or because of illnesses or drugs, bone is absorbed faster than it is made, the holes in the sponge enlarge and the bone becomes more brittle and likely to break. Things accelerating weakening include drugs such as steroids, a family history of osteoporosis, immobility, low oestrogen levels after the menopause, low testosterone levels, , smoking and excess alcohol. Recently, drugs suppressing oestrogen action in treatment of breast cancer can lead to bone thinning.
Of course, you cannot change your parents or age, but the other factors can be reviewed and may slow down or prevent increasing bone fragility. While being underweight is associated with low bone strength there is little evidence that dietary modifications influence osteoporosis. However weight bearing exercise such as walking, moderating alcohol consumption and giving up smoking all help. Indeed, the drugs used to increase bone strength are fighting a losing battle if other issues are not addressed.
Weak bones often only come to light because somebody sustains a fracture, like my patient, or because they are identified as being at high risk, for example through being treated with steroids.
One way of assessing bone strength is with a bone density scan. It is important to appreciate that bone density is a continuum and osteoporosis just one end of this scale. What matters is the overall risk of having a fracture and the bone density is just part of this. The scan examines one of the many features which influence bone strength but it is one that can be relatively easily measured and influenced with medication.
Having had a scan the need for treatment needs to be looked at in the context of the overall risk and all the other factors influencing bone strength mentioned above. In other words, not every osteoporosis needs to be treated, and conversely some who do not have it may still require treatment.
If a patient has a fracture because their bones are fragile most treatments for osteoporosis reduce a risk of future breaks by about 40%. While this means that a fracture can still occur even with treatment the chances of this happening are much reduced. On the other hand if your risk of having a fracture was low to start with, it is not worth having treatment to reduce that risk. For example, if your risk of having a fracture in the next 10 years is only 5%, it is not worth taking a drug for the next 5 years to reduce this risk to 3%.
How long a drug needs to be taken and possible side-effects need to be taken into account in deciding on treatment. However, a broken hip can be devastating, and the drugs used to treat osteoporosis are only very rarely associated with problems. If the risk of breaking a bone is high, the benefits of taking the drugs far outweigh the risks.
If treatment is required, most drugs act by slowing bone absorption rather than making new bone, and are typically taken for 3-5 years before assessing the need to continue. Too long a treatment can be associated with its own, albeit rare, problems. On average all drugs work equally well and the choice of which medication, if any, needs to be discussed with your doctor.
The success of treatment can be assessed by increases or even stability in the bone density on a further scan, or, best of all, by no more broken bones!
By Dr Malcolm Persey MD FRCP

ultant Rheumatologist, Royal Free London (Barnet & Chase Farm) http://www.rheumatology-malcolmpersey.co.uk secretary@drmalcolmpersey.com Secretary 07817255337 Appointments Kings Oak & Cavell BMI Hospitals 020 8370 9505 Bushey SPIRE 020 8901 5555 Royal Free Hadley Wood, Wellington Diagnostic & Outpatient & Waterfront Centres 07817255337